Abstract
Background
Laparoscopic pancreaticoduodenectomy (LPD), an advanced minimally invasive technique, has demonstrated advantages to open pancreaticoduodenectomy (OPD). However, this complex procedure requires a relatively long training period to ensure technical proficiency. This study was therefore designed to analyze the learning curve for LPD.
Methods
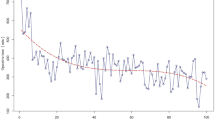
From October 2010 to September 2015, 63 standard pancreaticoduodenectomy procedures were to be performed laparoscopically by a single surgeon at the Department of Pancreatic Surgery, West China Hospital, Sichuan University, China. After applying the inclusion and exclusion criteria, a total of 57 patients were included in the study. Data for all the patients, including preoperative, intraoperative, and postoperative variables, were prospectively collected and analyzed. The learning curve for LPD was evaluated using both cumulative sum (CUSUM) and risk-adjusted CUSUM (RA-CUSUM) methods. All of the variables among the learning curve phases were compared.
Results
Based on the CUSUM and the RA-CUSUM analyses, the learning curve for LPD was grouped into three phases: phase I was the initial learning period (cases 1–11), phase II represented the technical competence period (cases 12–38), and phase III was regarded as the challenging period (cases 39–57). The operative time, intraoperative blood loss, and postoperative ICU demand significantly decreased with the learning curve. More lymph nodes were collected after the initial learning period. There were no significant differences in terms of postoperative complications or the 30-day mortality among the three phases. More challenging cases were encountered in phase III.
Conclusions
According to this study, the learning curve for LPD consisted of three phases. Conservatively, to attain technical competence for performing LPD, a minimum of 40 cases are required for laparoscopic surgeons with a degree of laparoscopic experience.




Similar content being viewed by others
References
de Wilde RF, Besselink MG, van der Tweel I, de Hingh IH, van Eijck CH, Dejong CH, Porte RJ, Gouma DJ, Busch OR, Molenaar IQ, Dutch Pancreatic Cancer G: Impact of nationwide centralization of pancreaticoduodenectomy on hospital mortality. Br J Surg 2012, 99: 404–10.
Balzano G, Zerbi A, Capretti G, Rocchetti S, Capitanio V, Di Carlo V: Effect of hospital volume on outcome of pancreaticoduodenectomy in Italy. Br J Surg 2008, 95: 357–62.
Yeo CJ, Cameron JL, Sohn TA, Lillemoe KD, Pitt HA, Talamini MA, Hruban RH, Ord SE, Sauter PK, Coleman J, Zahurak ML, Grochow LB, Abrams RA: Six hundred fifty consecutive pancreaticoduodenectomies in the 1990s: pathology, complications, and outcomes. Ann Surg 1997, 226: 248–57; discussion 57–60.
Jang JY, Kang MJ, Heo JS, Choi SH, Choi DW, Park SJ, Han SS, Yoon DS, Yu HC, Kang KJ, Kim SG, Kim SW: A prospective randomized controlled study comparing outcomes of standard resection and extended resection, including dissection of the nerve plexus and various lymph nodes, in patients with pancreatic head cancer. Ann Surg 2014, 259: 656–64.
Kneuertz PJ, Pitt HA, Bilimoria KY, Smiley JP, Cohen ME, Ko CY, Pawlik TM: Risk of morbidity and mortality following hepato-pancreato-biliary surgery. J Gastrointest Surg 2012, 16: 1727–35.
Seiler CA, Wagner M, Bachmann T, Redaelli CA, Schmied B, Uhl W, Friess H, Buchler MW: Randomized clinical trial of pylorus-preserving duodenopancreatectomy versus classical Whipple resection-long term results. Br J Surg 2005, 92: 547–56.
Gagner M, Pomp A: Laparoscopic pylorus-preserving pancreatoduodenectomy. Surg Endosc 1994, 8: 408–10.
Tran TB, Dua MM, Worhunsky DJ, Poultsides GA, Norton JA, Visser BC: The First Decade of Laparoscopic Pancreaticoduodenectomy in the United States: Costs and Outcomes Using the Nationwide Inpatient Sample. Surg Endosc 2015. doi: 10.1007/s00464-015-4444-y
Wang M, Zhang H, Wu Z, Zhang Z, Peng B: Laparoscopic pancreaticoduodenectomy: single-surgeon experience. Surg Endosc 2015, 29: 3783–94.
Croome KP, Farnell MB, Que FG, Reid-Lombardo K, Truty MJ, Nagorney DM, Kendrick ML: Total Laparoscopic Pancreaticoduodenectomy for Pancreatic Ductal Adenocarcinoma: Oncologic Advantages Over Open Approaches? Ann Surg 2014, 260: 633–40.
Song KB, Kim SC, Hwang DW, Lee JH, Lee DJ, Lee JW, Park KM, Lee YJ: Matched Case–control Analysis Comparing Laparoscopic and Open Pylorus-preserving Pancreaticoduodenectomy in Patients With Periampullary Tumors. Ann Surg 2015, 262: 146–55.
Speicher PJ, Nussbaum DP, White RR, Zani S, Mosca PJ, Blazer DG, 3rd, Clary BM, Pappas TN, Tyler DS, Perez A: Defining the learning curve for team-based laparoscopic pancreaticoduodenectomy. Ann Surg Oncol 2014, 21: 4014–9.
Kuroki T, Kitasato A, Adachi T, Tanaka T, Hirabaru M, Matsushima H, Soyama A, Hidaka M, Takatsuki M, Eguchi S: Learning Curve for Laparoscopic Pancreaticoduodenectomy: A Single Surgeon's Experience with Consecutive Patients. Hepatogastroenterology 2014, 61: 838–41.
Bokhari MB, Patel CB, Ramos-Valadez DI, Ragupathi M, Haas EM: Learning curve for robotic-assisted laparoscopic colorectal surgery. Surg Endosc 2011, 25: 855–60.
Park EJ, Kim CW, Cho MS, Baik SH, Kim DW, Min BS, Lee KY, Kim NK: Multidimensional analyses of the learning curve of robotic low anterior resection for rectal cancer: 3-phase learning process comparison. Surg Endosc 2014, 28: 2821–31.
American Joint Committee on Cancer (2010) AJCC cancer staging manual, 7th edn. Springer, New York.
Clavien PA, Barkun J, de Oliveira ML, Vauthey JN, Dindo D, Schulick RD, de Santibanes E, Pekolj J, Slankamenac K, Bassi C, Graf R, Vonlanthen R, Padbury R, Cameron JL, Makuuchi M: The Clavien-Dindo classification of surgical complications: five-year experience. Ann Surg 2009, 250: 187–96.
Bassi C, Dervenis C, Butturini G, Fingerhut A, Yeo C, Izbicki J, Neoptolemos J, Sarr M, Traverso W, Buchler M: Postoperative pancreatic fistula: an international study group (ISGPF) definition. Surgery 2005, 138: 8–13.
Wente MN, Bassi C, Dervenis C, Fingerhut A, Gouma DJ, Izbicki JR, Neoptolemos JP, Padbury RT, Sarr MG, Traverso LW, Yeo CJ, Buchler MW: Delayed gastric emptying (DGE) after pancreatic surgery: a suggested definition by the International Study Group of Pancreatic Surgery (ISGPS). Surgery 2007, 142: 761–8.
Wente MN, Veit JA, Bassi C, Dervenis C, Fingerhut A, Gouma DJ, Izbicki JR, Neoptolemos JP, Padbury RT, Sarr MG, Yeo CJ, Buchler MW: Postpancreatectomy hemorrhage (PPH): an International Study Group of Pancreatic Surgery (ISGPS) definition. Surgery 2007, 142: 20–5.
Wang X, Li Y, Crook N, Peng B, Niu T: Laparoscopic splenectomy: a surgeon's experience of 302 patients with analysis of postoperative complications. Surg Endosc 2013, 27: 3564–71.
Nomi T, Fuks D, Kawaguchi Y, Mal F, Nakajima Y, Gayet B: Learning curve for laparoscopic major hepatectomy. Br J Surg 2015, 102: 796–804.
Okrainec A, Ferri LE, Feldman LS, Fried GM: Defining the learning curve in laparoscopic paraesophageal hernia repair: a CUSUM analysis. Surg Endosc 2011, 25: 1083–7.
Bege T, Lelong B, Esterni B, Turrini O, Guiramand J, Francon D, Mokart D, Houvenaeghel G, Giovannini M, Delpero JR: The learning curve for the laparoscopic approach to conservative mesorectal excision for rectal cancer: lessons drawn from a single institution's experience. Ann Surg 2010, 251: 249–53.
Song MH, Kuwabara F, Ito T: Risk-adjusted mortality rate cumulative sum analysis based on the Japan SCORE represents a learning curve in mitral valve reparative surgery. Surg Today 2014, 44: 1253–7.
Kim HJ, Choi GS, Park JS, Park SY: Multidimensional analysis of the learning curve for robotic total mesorectal excision for rectal cancer: lessons from a single surgeon's experience. Dis Colon Rectum 2014, 57: 1066–74.
Son G-M, Kim J-G, Lee J-C, Suh Y-J, Cho H-M, Lee Y-S, Lee I-K, Chun C-S: Multidimensional Analysis of the Learning Curve for Laparoscopic Rectal Cancer Surgery. Journal of Laparoendoscopic & Advanced Surgical Techniques 2010, 20: 609–17.
Dokmak S, Fteriche FS, Aussilhou B, Bensafta Y, Levy P, Ruszniewski P, Belghiti J, Sauvanet A: Laparoscopic pancreaticoduodenectomy should not be routine for resection of periampullary tumors. J Am Coll Surg 2015, 220: 831–8.
Bailey MB, Davenport DL, Vargas HD, Evers BM, McKenzie SP: Longer operative time: deterioration of clinical outcomes of laparoscopic colectomy versus open colectomy. Dis Colon Rectum 2014, 57: 616–22.
Boggi U, Amorese G, Vistoli F, Caniglia F, De Lio N, Perrone V, Barbarello L, Belluomini M, Signori S, Mosca F: Laparoscopic pancreaticoduodenectomy: a systematic literature review. Surg Endosc 2015, 29: 9–23.
Marusch F, Gastinger I, Schneider C, Scheidbach H, Konradt J, Bruch HP, Kohler L, Barlehner E, Kockerling F, Laparoscopic Colorectal Surgery Study G: Experience as a factor influencing the indications for laparoscopic colorectal surgery and the results. Surg Endosc 2001, 15: 116–20.
Tekkis PP, Senagore AJ, Delaney CP, Fazio VW: Evaluation of the learning curve in laparoscopic colorectal surgery: comparison of right-sided and left-sided resections. Ann Surg 2005, 242: 83–91.
Larach SW, Patankar SK, Ferrara A, Williamson PR, Perozo SE, Lord AS: Complications of laparoscopic colorectal surgery. Analysis and comparison of early vs. latter experience. Dis Colon Rectum 1997, 40: 592–6.
Valsangkar NP, Bush DM, Michaelson JS, Ferrone CR, Wargo JA, Lillemoe KD, Fernandez-del Castillo C, Warshaw AL, Thayer SP: N0/N1, PNL, or LNR? The effect of lymph node number on accurate survival prediction in pancreatic ductal adenocarcinoma. J Gastrointest Surg 2013, 17: 257–66.
Huebner M, Kendrick M, Reid-Lombardo KM, Que F, Therneau T, Qin R, Donohue J, Nagorney D, Farnell M, Sarr M: Number of lymph nodes evaluated: prognostic value in pancreatic adenocarcinoma. J Gastrointest Surg 2012, 16: 920–6.
Cai Y, Peng B, Mai G, Ke N, Liu X: Laparoscopic distal pancreatectomy for solid-pseudopapillary tumor of the pancreas. Surg Laparosc Endosc Percutan Tech 2015, 25: e8-e10.
Wang MJ, Li JL, Zhou J, Wu Z, Peng B: Consecutive laparoscopic gallbladder and spleen resections in cirrhotic patients. World J Gastroenterol 2014, 20: 546–54.
Acknowledgments
The West China Hospital, Sichuan University funded this study.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Disclosure Statement
The authors have no competing financial interests to report.
Conflicts of Interest
The authors declare that they have no conflicts of interest.
Additional information
Zhaoda Zhang and Bing Peng contributed equally to this work.
Rights and permissions
About this article
Cite this article
Wang, M., Meng, L., Cai, Y. et al. Learning Curve for Laparoscopic Pancreaticoduodenectomy: a CUSUM Analysis. J Gastrointest Surg 20, 924–935 (2016). https://doi.org/10.1007/s11605-016-3105-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11605-016-3105-3